“Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”1-The Robert Wood Johnson Foundation. Health equity or inequity reflects social vulnerabilities and inequalities where people live, work, play, and worship. These social vulnerabilities and inequities impact colorectal cancer (CRC) outcomes and mortality.
vulnerable groups
|
Populations experiencing conditions such as poverty, disability, and housing insecurity– factors that can have a negative effect on health2 Examples Include: |
|
Individuals facing financial insecurity |
Rural residents, who often encounter |
|
People without access to transportation |
Elderly individuals |
|
Members of certain racial and ethnic groups |
People with other chronic health conditions, |
|
Individuals without insurance, |
Members of the LGBTQ+ community |
|
People experiencing homelessness or living in unsafe or crowded housing |
|
Social determinants of health
|
Conditions in the environments in which people are born, live, learn, work, play, worship, and age. These factors influence health, functioning, and quality-of-life outcomes3
Examples Include: |
|
Economic Stability |
concentrated poverty, economic opportunity, literacy |
| Education |
high school graduation, completion of higher education, |
| Social and Community Context |
distrust of the government, social support |
| Health and Healthcare |
access to healthcare, health literacy |
|
Neighborhood and Built Environment |
food desserts, sanitation services, |
| Factors of influence:
discrimination, racism, residential segregation, social disorder |
|
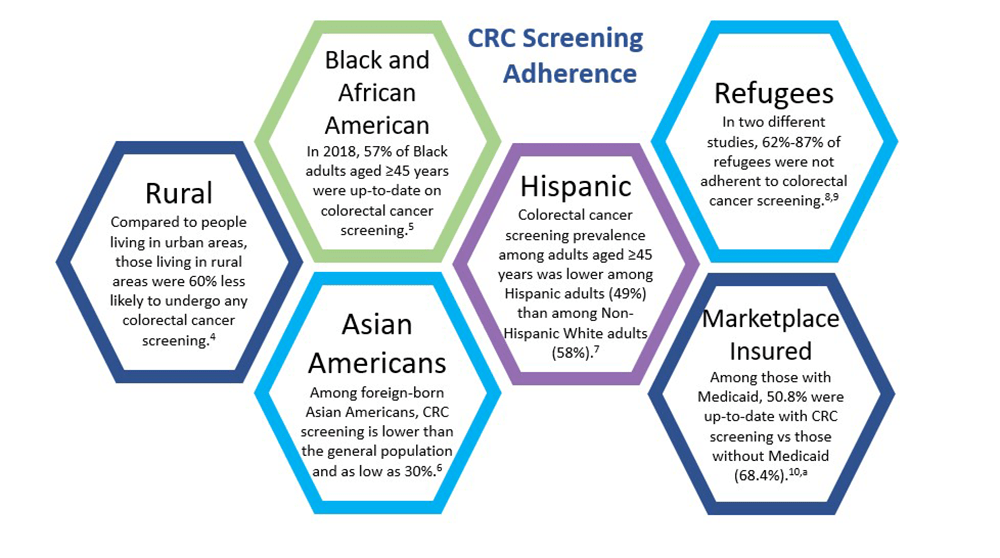
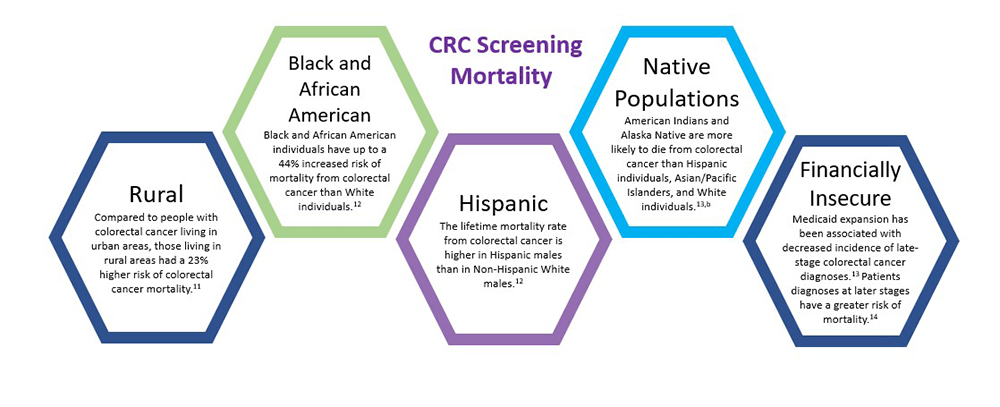
Social vulnerabilities and health inequalities affect Colorectal Cancer (CRC) Screening in a variety of ways
Last Updated: 4/8/2023
References
1 Braveman P, Arkins E, Orleans T, et al. What is health equity? Published May 2017. Accessed January 12, 2023. https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html
2 Agency for Toxic Substances and Disease Registry. CDC/ATSDR Social vulnerability index (SVI). Updated November 16, 2022. Accessed January 12, 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
3 Office of Disease Prevention and Health Promotion. Social determinants of health. Updated February 6, 2022. Accessed January 12, 2023. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
4 Alyabsi M, Meza J, Islam KMM, et al. Colorectal cancer screening uptake: differences between rural and urban privately-insured population. Front Public Health. 2020. Published Online First on November 19,2020. doi:10.3389/fpubh.2020.532950
5 Gan T, Sinner HF, Walling SC, et al. Impact of the Affordable Care Act on colorectal cancer screening, incidence, and survival in Kentucky. J Am Coll Surg. 2019;228(4):342-353.e1
6 Kim K, Chandrasekar E, Lam H. Colorectal cancer screening among Chinese, Cambodian, and Vietnamese immigrants in Chicago. J Racial Ethn Health Disparities. 2015;2(4):473-480
7 ACS. Cancer Facts & Figures for Hispanics/Latinos 2021-2023. Atlanta: American Cancer Society. 2021
8 Milenkov A, et al. Uptake of cancer screenings among a multiethnic refugee population in North Texas, 2014-2018. PLoS One. 2020. Published Online First on March 30,2020. doi:10.1371/journal.pone.0230675
9 Siddiq H, Alemi Q, Mentes J, et al. Preventive cancer screening among resettled refugee women from Muslim-majority countries: a systematic review. J Immigr Minor Health. 2020;22(5):1067-1093
10 Gangcuangco LMA, Rivas T, Basnet A, et al. Factors associated with colorectal cancer screening adherence and the impact of COVID-19 on screening patterns in Connecticut, USA. Intern Emerg Med. 2022;17(8):2229-2235.
11 CDC. An update on cancer deaths in the United States. Updated February 28, 2022. Accessed cited January 12, 2023. https://www.cdc.gov/cancer/dcpc/research/update-on-cancer-deaths/index.htm
12 Siegel RL, Miller KD, Wagle NS. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48
13 Melkonian SC, Weir HK, Jim MA, et al. Incidence of and trends in the leading cancers with elevated incidence among American Indian and Alaska Native populations, 2012 -2016. Am J Epidemiol. 2021;190(4):528-538.
14 Primm KM, Huepenbecker SP, Zhao H, et al. Impacts of Medicaid expansion on stage at cancer diagnosis by patient insurance Type. Am J Prev Med. 2022;63(6):915-925.Braveman P, Arkins E, Orleans T, et al. What is health equity? Published May 2017. Accessed January 12, 2023. https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html
Footnotes
a Data based on a study of 12,189 patients receiving care in Connecticut; the study included patients aged 50-75 years, and therefore does not represent the full screening eligible population of people ≥45.
b Note that the AI/AN population has the highest racial misclassification in health data of any racial or ethnic group in the U.S., likely contributing to an underestimation of the burden of cancer among members of this group.