A number of genetic mutations are associated with increased risk for colorectal cancer (CRC), and genetic variants seem to play a role in young-onset disease. Overall, genetic variants drive ~20% of cases of CRC in patients <50 years of age. According to recent data, among this age group, 13% of pathogenic variants are associated with Lynch Syndrome or polyposis syndromes. It is important to note that the majority of patients with young-onset disease do not have a genetic predisposition for CRC.1
PREVALENCE OF PATHOGENIC VARIANTS BY AGE AT CRC DIAGNOSIS1,a

- Younger patients have an increased prevalence of germline variants1
- Guidelines recommend multigene panel testing of all young patients with CRC1
| Genes That Contain Pathogenic Variants1 | |||
|---|---|---|---|
| OTHER PATHOGENIC VARIANTS (5%) | |||
| LYNCH SYNDROME (10%) |
POLYPOSIS SYNDROMES (3%) |
HIGH PENETRANCE |
MODERATE / LOW PENETRANCE |
| MLH1 | APC | BRCA1 | CHEK2 |
| MSH2 | MUTYH | BRCA2 | ATM |
| MSH6 | SMAD4 | TP53 | NBN |
| PMS2 | BMPR1A | PALB2 | BARD1 |
| PTEN | CDKN2A | BRIP1 | |
| POLE | |||
- An increased risk for CRC is linked to germline variants in several genes1
- Up to 10% of patients with CRC have germline variants in genes that have been linked to moderate or high cancer risk1
PATHOGENESIS: GENETIC AND EPIGENETIC EVENTS2
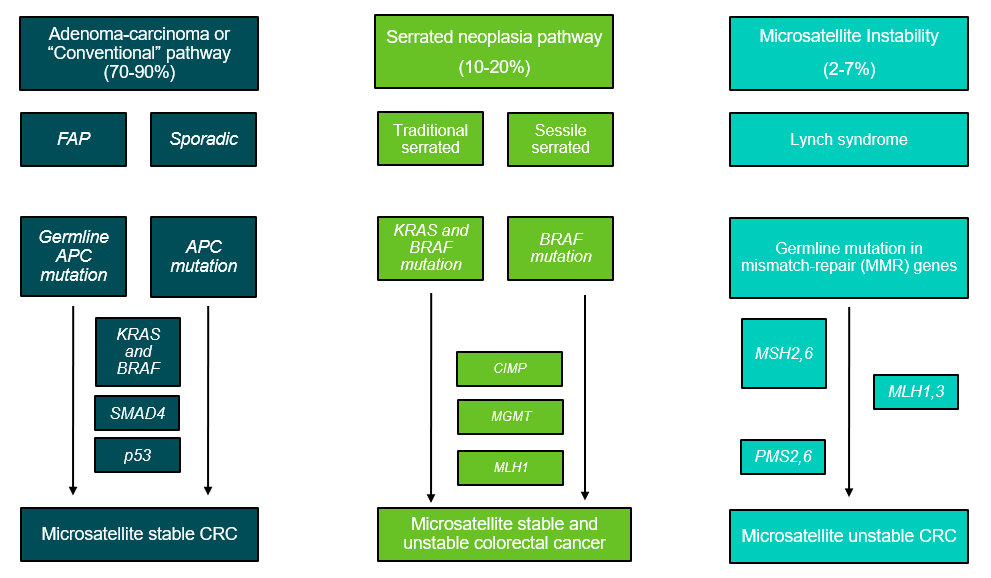
- Adenoma-carcinoma, or the conventional pathway, accounts for 70-90% of CRC cases, which can develop sporadically or due to familial adenomatous polyposis2
- The serrated neoplasia pathways accounts for 10-20% of cases, while microsatellite instability is related to 2-7% of CRC cases2
- Learn more about the pathobiology of CRC
FAP: familial adenomatous polyposis, CRC: colorectal cancer, APC: Adenomatous polyposis coli, KRAS: Kirsten rat sarcoma viral oncogene homolog, BRAF: B-Raf proto-oncogene serine/threonine kinase, SMAD4: SMAD family member 4, MGMT: methyl-guanine-DNA-methyltransferase, MLH: MutL Homolog, MSH: Mut S homologue, PMS: postmeiotic segregation increased
References
1 Stoffel, EM, Murphy CC. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterol. 2020;158:341–353.
2 Dekker E, Tanis PJ, Vleugels J, et al. Colorectal cancer. Lancet. 2019;394:1467–1480.
Footnotes
a Pie charts do not consistently add to 100%1
Last Updated: 3/13/2023