Risk factors for colorectal cancer (CRC) are categorized as either modifiable or nonmodifiable. Nonmodifiable risk factors include age and personal or family history of CRC. Personal or family history of CRC is considered to be associated with a high risk of developing CRC. Modifiable risk factors include many health and wellness related factors and are generally associated with an increased risk of CRC. In general, over half of all CRC is attributable to modifiable lifestyle factors.1-6
ASYMPTOMATIC PATIENTS ARE GENERALLY CONSIDERED TO BE AT AVERAGE RISK FOR CRC IN THE ABSENCE OF: 1-5
A personal history of:
- CRC, adenomatous polyps, or IBD (including Crohn’s disease and ulcerative colitis)
- Radiation to the abdomen/pelvic area to treat prior cancera
- Cystic fibrosis and a confirmed or suspected high-risk CRC genetic syndromes (such as familial adenomatous polyposis or Lynch syndrome)
A family history of:
- First degree relative who has had CRC or advanced lesions
- Familial adenomatous polyposisb
- Hereditary CRC syndrome
Each Patient’s Risk Must be Assessed Individually
Consider These Risk Factors When Screening Patients for CRC
The presence of these risk factors alone does not elevate patients beyond the average-risk category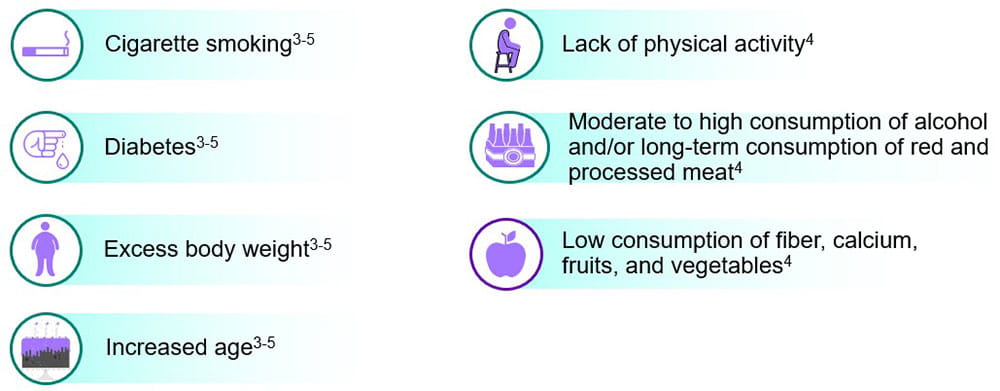
- Having a 1 or more first degree relatives with CRC is associated with an increased or high risk for the development of CRC2
- This risk is further increased when first degree relatives with CRC are under the age of 50 years2
- Certain factors associated with Western lifestyles are known to increase the risk of developing CRC
- While assessment of these factors provides an important opportunity for lifestyle modification advice, their presence is not considered sufficient to elevate individuals beyond the average-risk category, and there is no evidence to support their use in stratifying subgroups of the population within the average-risk category4,5
- In the United States, ~55% of all CRCs are attributable to modifiable lifestyle factors2
| Factors That Increase Risk | Relative Riske |
|
Hereditary and medical history |
|
| Family history of CRC | |
|
1 or more first-degree relatives |
2.2 |
|
1 or more first-degree relatives diagnosed |
3.6 |
|
2 or more first-degree relatives |
4.0 |
|
1 or more second-degree relatives |
1.7 |
| Inflammatory bowel disease | 1.7 |
| Type 2 diabetes | |
|
Male |
1.4 |
|
Female |
1.2f |
| Modifiable Factors | |
| Heavy alcohol (daily average >3 drinks) | 1.3 |
| Obesity (Body Mass Index ≥30 kg/m2) | 1.3 |
| Colon Male | 1.5 |
| Female | 1.1 |
| Rectum Male | 1.3 |
| Female | 1.0 |
| Red meat consumption (100 g/day) | 1.1 |
| Processed meat consumption (50 g/day) | 1.2 |
| Smoking (current vs. never) | |
| Proximal colon | 1.2 |
|
Distal colon |
1.1 |
| Rectum | 1.3 |
| Factors that decrease risk: | |
| Physical activity (colon) | 0.7 |
| Dairy consumption (400 g/day) | 0.9 |
- People with a first-degree relative (parent, sibling, or child) diagnosed with CRC have 2 to 4 times the risk of developing CRC, making timely screening critical in this population.2 Both a history of a distant relative and a family history of adenomas also increase the risk of developing CRC but to a lesser degree.2
- Obesity, inactivity, smoking, heavy alcohol use, and high consumption of red or processed meat may also be considered when estimating CRC risk for individual patients.2,5
CRC: Colorectal Cancer, FAP: Familial Adenomatous Polyposis, IBD: Inflammatory Bowel Disease (Ulcerative Colitis, Crohn’s Disease)
References
1 PDQ Screening and Prevention Editorial Board. PDQ colorectal cancer prevention. Bethesda, MD: National Cancer Institute. Updated March 29, 2021. Accessed May 30, 2023. https://www.cancer.gov/types/colorectal/hp/colorectal-prevention-pdq
2 American Cancer Society. Colorectal cancer facts & figures 2023-2025. Atlanta: American Cancer Society; 2023
3 Davidson KW, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977.
4 Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68(4):250-281.
5 Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017;112(7):1016-1030.
6 Gupta S, Lieberman D, Anderson JS, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterol. 2020;158(4):1131-1153.e5.
7 Hahn EE, Gould MK, Munoz-Plaza CE, et al. Understanding comorbidity profiles and their effect on treatment and survival in patients with colorectal cancer. J Natl Compr Canc Netw. 2018;16(1):23-34.
8 Fu AZ, Zhao Z, Gao S, et al. Comorbid conditions in patients with metastatic colorectal cancer. World J Oncol. 2011;2(5):225-231.
Footnotes
a ACS guideline excludes patients with radiation to the abdomen/ pelvic area to treat prior cancer from the average-risk category.
b Polyposis syndromes: classical familial adenomatous polyposis (FAP), attenuated FAP (AFAP), MUTYH-associated polyposis (MAP), Peutz-Jeghers syndrome (PJS), juvenile polyposis syndrome (JPS), serrated polyposis syndrome (SPS), rare genetic causes of multiple adenomatous polyps.
c Retrospective, observational cohort study using longitudinal data from the Kaiser Permanente Southern California (KPSC) system. Latent class analysis (LCA) was used to identify comorbidity profiles of 7803 patients ages of 18 to 64 at diagnosis of CRC between January 1, 2008, and December 31, 2013. The EHR was used to identify treatment received and used Cox proportional hazards analysis to examine the effect of comorbidity class on survival, as well as the effect of comorbidity profile on receipt of guideline-recommended treatment.
d This retrospective cohort study was conducted in a population of patients 18 or older with newly diagnosed metastatic colorectal cancer (mCRC). Data was sourced from linked medical and pharmacy claims data between January 2005 and June 2008 from two US-based Medstat MarketScan claims databases. Data was analyzed for comorbid conditions and medication use in the year prior to diagnosis of mCRC. Limitations include the fact that comorbidities were identified based on healthcare service use data, thus comorbid conditions that did not trigger healthcare service use prior to diagnosis were not captured. In addition, history of smoking and obesity rates were very low, likely due to under-reporting of these two conditions in claims databases. Univariate analyses were conducted to compare the comorbid conditions between patients aged ≥65 and <65 years old. In total, 12,648 patients aged ≥18 years were identified. The study was evenly populated by gender and age above and below 65, and most patients had a primary diagnosis of colon cancer (70.1%).
e The risk of disease in people with a particular “exposure” compared to people without the exposure. For dietary factors the highest versus lowest consumption is compared. A value greater than 1 indicates higher risk with exposure, whereas less than 1 is a protective effect.
f The association was not statistically significant.
Last Updated: 5/30/2023